Cardiology
Thanks to our interdisciplinary team and the joint definition of your rehabilitation goals, we are demonstrably able to extend your lifespan, minimize the burden of your illness and thus improve your quality of life. They should be able to participate in all areas of life again. Our aim is to make you an expert on your illness. If you know what to look out for, you will also know what you can be confident about. Our core element is the “Poly-Pill” movement.
Doctor
We are here for you
- After a heart attack
- After heart bypass surgery
- For coronary heart disease with stable angina pectoris
- After balloon dilatation/stent implantation
- After heart valve surgery
- For cardiac insufficiency (heart failure)
- After implantation of pacemaker, defibrillator (ICD), CRT
- For heart muscle diseases (cardiomyopathies) such as myocarditis
- After expired pulmonary embolism
- Diseases of the arterial vessels (aorta, neck, pelvic and leg vessels) with stenting or bypass surgery
- For cardiac arrhythmias such as atrial fibrillation
- For metabolic syndrome with
- High blood pressure
- Diabetes mellitus
- Fat metabolism disorder
- Overweight and obesity
Disease patterns and therapy
An incisive event. The maximum form of arteriosclerosis is occlusion of the coronary arteries. Time is running out. The vessel must be reopened as quickly as possible to prevent cardiac arrhythmia and heart failure. This is done either in the cardiac catheterization laboratory by means of balloon dilatation and stenting or a heart bypass operation. Now you need to restore both your physical and mental strength. We in the rehabilitation department specialize in wound and pain management as well as physiotherapeutic exercise. Through daily supervised training, your fitness increases and you regain confidence in your own body. This is supported by a separate specialist department, psychocardiology. All 10 risk factors for arteriosclerosis are individually optimized. The core element is the “Poly-Pill” movement. We want to make you experts in your disease, which is why we also offer a variety of lectures. Our multimodal rehabilitation follows the current guidelines. Several studies have shown that cardiac rehabilitation extends your lifespan. It also helps to avoid further hospital stays and improves your quality of life.
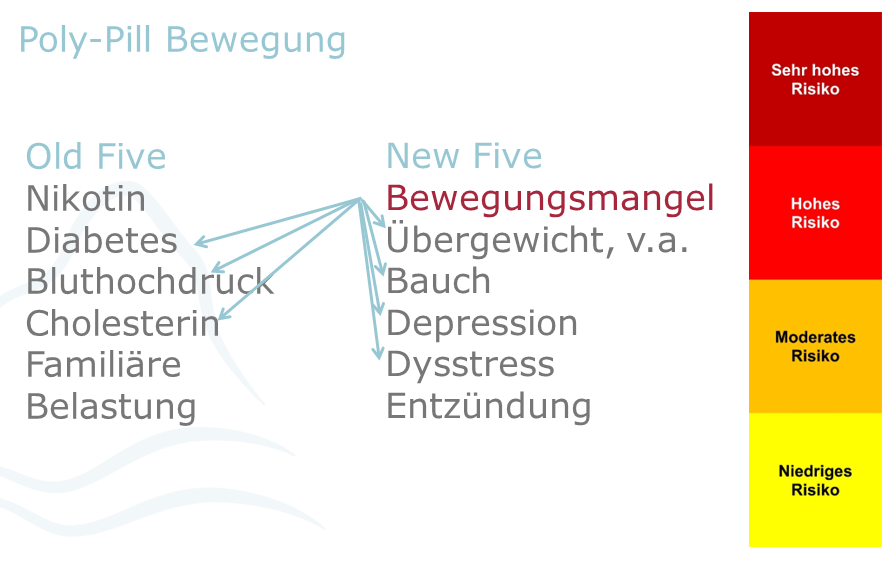
It is the main manifestation of vascular calcification (arteriosclerosis). Arteriosclerosis in the heart means a heart attack, arteriosclerosis in the head means a stroke and arteriosclerosis in the leg means arterial occlusive disease. There is no such thing as simply “pipe-free”. However, we know very well that we can stop the progression of arteriosclerosis by optimally adjusting the 10 risk factors. Both the well-known “old five” risk factors and the newly recognized “new five-even bigger” risk factors are treated, above all through the “poly-pill” movement. A certified nicotine-free seminar and interactive lectures round off the individual adjustment of the therapy in individual visits.
The disease (anatomy, frequency)
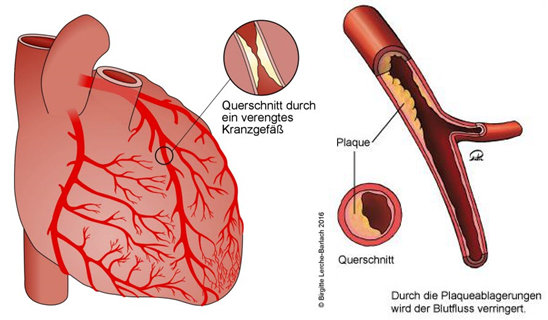
CHD is characterized by constrictions or occlusions of the coronary arteries, which are responsible for blood flow to the heart. This is due to deposits, so-called plaques, which consist of cholesterol, other fats, inflammatory cells and connective tissue. The diameter of a blood vessel slowly but steadily decreases. If the blood flow is severely reduced (ischemia), the heart muscle is no longer supplied with sufficient oxygen and nutrients. At the same time, metabolic waste products accumulate. The causes of the development and progression of CHD are not yet fully understood. It is clear that, in addition to a predisposition to the disease (hereditary component), lifestyle plays an important role: Smoking, lack of exercise and obesity are significant risk factors. An undetected and untreated high cholesterol level, high blood pressure and diabetes also increase the risk of developing CHD.
In Germany, 6 million people suffer from CHD.
Complaints
One of the most important symptoms of CHD is chest tightness (angina pectoris). Initially, symptoms occur under physical stress, later also for no apparent reason. The symptoms can radiate into the neck or jaw area, the back, the shoulder or the abdomen. Shortness of breath and/or shortness of breath can also be signs of CHD. The symptoms often occur during physical exertion, for example when walking fast or climbing stairs, and then disappear again when the exertion is over – this is a stable situation, the so-called stable angina pectoris (= CCS, chronic coronary syndrome)
However, if the symptoms occur at rest (unstable angina pectrois), e.g. at night in bed, this is a warning sign: This form is particularly dangerous as a possible harbinger of a heart attack. If our coronary arteries become completely blocked, the heart muscle can no longer be supplied with sufficient oxygen. In this case, you should call for medical help immediately (call 112).
Diagnostics
If the doctor suspects the presence of CHD, he/she will carry out various tests on you, in particular an electrocardiogram (ECG), blood pressure measurement, blood and metabolic tests or a cardiac ultrasound (ECHO). The most accurate way to detect CHD is with a cardiac catheterization.
Treatment
What can those affected do?
- Daily exercise (e.g. cycling, walking, dancing or swimming) will keep your heart fit, even if you already have CHD.
- In addition to exercise, you should make sure you eat a healthy diet: We recommend lots of fruit and vegetables, but little meat and convenience products. A typical heart-healthy diet is the so-called Mediterranean diet, which is rich in olive oil, nuts, sea fish, fruit and vegetables.
- You should not smoke even in old age – smoking damages your own heart, but also the heart and the health of those around you through passive smoking. Try to stop smoking.
- Avoid drinking alcohol, especially if you are taking medication.
- The medication can only work properly if you take it as prescribed by a doctor.
- If you experience severe heart problems, shortness of breath or unconsciousness, do not hesitate to call for medical help.
Treatment options
Drug therapy is the basis of treatment for all patients with CHD. As a rule, the medication must be taken long-term.
- Anticoagulants prevent blood platelets from sticking to the walls of the coronary arteries. People with CHD are usually given acetylsalicylic acid – known as ASA.
- Statins ensure favorable blood lipid levels. This means that fewer plaques accumulate on the inside of the vessels.
Beta-blockers, ACE inhibitors and other medications can also be used permanently for certain clinical pictures.
For sudden symptoms outside of a heart attack, nitrates such as nitro spray or nitro capsules or ranolazine can help temporarily. If medication does not succeed in controlling the symptoms or if examinations indicate a pronounced CHD with multiple constrictions or occlusions, doctors have two further options for opening (revascularizing) vessels.
You can insert vascular stents using a cardiac catheter. These are small tubes made of wire mesh that are inserted into a container to keep it open.
If several vessels are affected or if the constrictions are unfavorable for a stent, European guidelines advocate bypass surgery. Constrictions are then bridged by additional blood vessels (bypass).
Rehab and AHB (requirements, benefits)
After acute coronary syndrome (ACS): Whether after a cardiac catheterization procedure or aortocoronary bypass surgery with an uncomplicated course, rehabilitation should begin after just a few days, as this significantly reduces mortality and further hospital stays (morbidity).
In the case of chronic coronary syndrome (CCS): cardiac rehabilitation should also be carried out, as this significantly reduces mortality and morbidity. Patients with
- limited prognosis due to inadequately controlled cardiovascular risk factors
- persistent and limiting cardiac symptoms (angina pectoris and/or dyspnea) without the possibility of coronary revascularization (restoration of vascular perfusion)
- concomitant diseases that increase the risk of an unfavorable course of CCS, such as peripheral arterial occlusive disease (paVK), COPD, diabetes mellitus or chronic kidney disease.
- Endangerment or already existing restriction of professional and/or private participation as a result of CCS.
The benefits of AHB / rehab are
According to the guideline*, cardiac rehab has a positive influence on the following points:
- additional lifetime (reduction in mortality) as the scientifically “hardest” endpoint
- non-fatal re-infarctions
- non-fatal strokes
- Repeated hospital admissions/stays
- the individual, health-related quality of life
The risks in the course after acute coronary heart disease (e.g. renewed or persistent myocardial ischemia, stent occlusion or restenosis, myocardial insufficiency and arrhythmias) are known. Cardiac rehabilitation is therefore responsible for the close medical care of patients with timely detection and treatment of such risks. Drug therapy and, in particular, the necessary lifestyle changes with physical training continue to be of central importance in cardiac rehabilitation. In addition to improving the clinical prognosis, these measures also aim to ensure or restore individual quality of life and social integration (participation) in the long term.
*Guideline on cardiac rehabilitation (LL-KardReha, DACH 2020) in German-speaking Europe Germany, Austria, Switzerland
Typical rehabilitation goals
- Assessment of physical resilience (recognizing alarm signals and the limits of the body)
- Increasing the walking distance on a flat surface with/without a rollator
- Improved performance when climbing stairs (number of floors)
- Information on CHD, high blood pressure, dealing with anxiety, learning to deal with your own vulnerability
- Minimization of risk factors (setting cholesterol levels, blood sugar, blood pressure, dysstress, abdominal fat, nicotine, lack of exercise)
- Smoking cessation / “What are the benefits of not smoking?”
- Psycho-mental stabilization, learning relaxation methods
- Improvement of difficulty falling asleep / sleeping through the night
- Improvement of wound healing
- Improvement of the pain situation
Therapy at the GZO
- Diagnostics (specialist visits, resting ECG, echocardiography, wound assessment, blood count, stress ECG, blood count)
- Optimization of pharmacotherapy (drug adjustment of blood coagulation, blood lipid levels, pumping performance, stress reaction of the heart)
- Physical training mainly in the form of aerobic endurance training using the endurance or interval method (ergometer cardiovascular training, terrain training or Nordic walking, group gymnastics and everyday training, medical training therapy)
- Knowledge transfer about the disease Basics for understanding CHD, its development (cardiovascular risk factors, risk behavior and risk diseases), its consequences and treatment options. In addition, training courses on hypertension, arteriosclerosis, disease management, measurement of blood coagulation and lipid metabolism
- Nutritional advice A typical heart-healthy diet is the so-called Mediterranean diet, which is rich in olive oil, nuts, sea fish, fruit and vegetables. Nutritional counseling is available in the form of individual counseling, group counseling and a training kitchen.
- Social care and prescription of medical aids
Psychological counseling and therapy (learning relaxation methods such as PMR, imagination, Qi Gong; individual and group sessions if required)
What happens at home?
In order to seamlessly maintain what has been achieved in the rehabilitation clinic (phase II rehabilitation), we arrange a heart group (phase III rehabilitation) as an outpatient aftercare program
- Moderate endurance training in the THF range (training heart rate), ideally 5×30 min or 3×50 min supplemented by a cardio group, plus moderate strength training and coordination 2-3 times a week
- Participation in “Disease Management” programs (DMP) for coronary heart disease. These are structured GP treatment programs for chronically ill people. The aim is to coordinate and optimize the treatment and care processes of patients over the entire course of their illness and across the boundaries of the individual service providers (GP, specialist, physiotherapy).
After balloon dilatation/stent implantation
Balloon dilatation/stent implantation is a treatment option for arteriosclerosis.
After heart bypass surgery (link to KHK)
Cardiac bypass surgery is a treatment option for arteriosclerosis.
After heart valve surgery
The most common valve disease is aortic valve stenosis (narrowing), followed by mitral valve insufficiency (leakage). Both valves belong to the left ventricle, which supplies the body’s circulation with oxygen-rich blood. If aortic valve stenosis or mitral valve insufficiency progresses, this can lead to heart failure, as the heart muscle has to do more work than intended. Cardiac arrhythmia can also be the result.
Three methods are available for both flaps:
- Invasive, i.e. through open surgery,
- non-invasive through catheter procedures,
- minimally invasive using endoscopy technology.
The ideal procedure is determined in advance by the heart team, consisting of cardiologists, cardiac surgeons and anesthesiologists, in a “valve conference”.
Thanks to our INCREASE research project (optimized pre-, intra- and post-operative rehabilitative care of valve patients) in cooperation with Augsburg University Hospital, we have maximum expertise for all heart valve diseases.
Aortic valve stenosis is described below as an example.
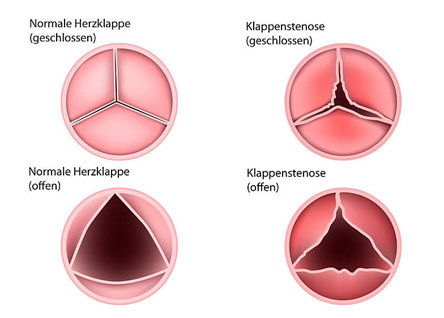
As one of a total of four heart valves, the aortic valve performs an important function in our body. It is located between the left ventricle and the aorta. There it acts as an outlet valve: with every heartbeat it only allows oxygen-rich blood to flow in the direction of the aorta. The valve closes between the beats in the relaxation phase of the heart (diastole) and thus prevents the blood from flowing back into the ventricle. The flap consists of three pockets, which in turn are made of delicate connective tissue.
If deposits of calcium, cholesterol and inflammatory cells lead to narrowing of the pockets, this is known as aortic valve stenosis. The pockets thicken, lose mobility – and become tight. The valve thus becomes an obstacle to the blood flow – and the heart muscle is put under too much strain because it has to do more than it should. The pumping capacity then also decreases in the further course. Aortic valve stenosis usually develops with age.
Aortic valve stenosis is now the third most common cardiovascular disease in Europe after high blood pressure (arterial hypertension) and coronary heart disease. The disease occurs more frequently with increasing age. Among the over-75s, 3-5% of people are affected.
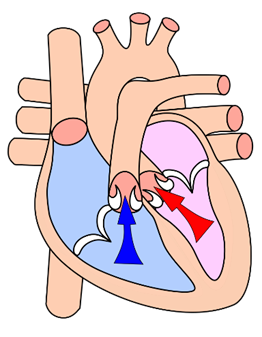
Outflow tract of the left ventricle
Complaints
Symptoms such as shortness of breath, a feeling of pressure in the chest, dizziness, reduced performance and fainting normally occur during physical exertion. If aortic valve stenosis is not treated, symptoms can occur over time even at rest. In the long term, severe functional impairment of the aortic valve shortens the patient’s lifespan.
Treatment options
What can those affected do?
In the case of mild to moderate stenosis, the patient should maintain a healthy lifestyle and minimize risk factors such as obesity, lack of exercise and high blood pressure.
Surgical procedures
If the narrowing is already very pronounced, it must be treated surgically. The calcified heart valve can be surgically removed (via a chest wall incision on the open heart) by a heart surgeon and an artificial (biological or mechanical) heart valve can be sewn in. To gain access to the heart, the surgeon cuts through the breastbone (sternum) in the classic procedure.
Each of these procedures usually requires the use of a heart-lung machine and general anesthesia. The heart is temporarily “immobilized”, the narrowed aortic valve is removed and replaced with a new one. Mechanical or biological replacement flaps can be used for this purpose.
The mechanical valves last a lifetime, but also require lifelong and strict medication to inhibit blood clotting (anticoagulation) in order to avoid the risk of blood clots. Biological valves made from bovine or porcine pericardial tissue do not require lifelong anticoagulation, but only last around 10 to 20 years (with considerable individual variance).
Minimally invasive surgery is regarded as a new and pioneering procedure. Here, the sternum is opened only 5 cm or not at all.
Catheter-assisted aortic valve replacement (TAVI)
For some time now, valve replacement can also be performed non-invasively without surgery using catheter technology. Patients usually have less pain after the procedure and become mobile again more quickly.
The procedure, also known as TAVI, stands for Transcatheter Aortic Valve Implantation. This has revolutionized the treatment of aortic valve stenosis and is now a standard procedure for patients at medium and high risk. The new heart valve is first attached to a special catheter and pushed into the narrowed heart valve via various access routes that only require a small incision. By far the most common access route is via the inguinal artery (femoral/transfemoral artery).
The replacement valve is always a biological prosthesis made of bovine or porcine pericardial tissue, anchored in a wire mesh. According to current knowledge, TAVI valves have a similar longevity to biological heart valves implanted by conventional surgery. The procedure via the inguinal artery does not require general anesthesia. The use of a heart-lung machine is also not necessary. The heart valves implanted with the catheter can also be implanted into previously implanted biological heart valves – i.e. heart valve within heart valve. This procedure is then called the “valve-in-valve procedure”.
A combination of minimally invasive surgery and catheter-based procedures are now also in use.
Rehab and AHB (requirements, benefits)
After an aortic valve operation, a 3-week rehabilitation period (follow-up treatment) is the rule, i.e. rehabilitation immediately or a maximum of two weeks after hospitalization.
As aortic valve stenosis is a degenerative heart valve disease that develops over many years, it does not only affect the heart. The whole organism has adapted to the resulting reduction in cardiac output. Once the diseased aortic valve has been repaired, it often takes several months for the body to reach its full, improved performance capacity in line with the restored capabilities of the heart.
In rehab, this process is trained and the body can carefully learn to approach the new possibilities under medical supervision and guidance.
Typical rehabilitation goals
- Assessment of physical resilience (recognizing alarm signals and the limits of the body)
- Increasing the walking distance on a flat surface with / without a rollator
- Improved performance when climbing stairs (number of floors)
- Information on the heart valve, dealing with anxiety
- Minimization of risk factors (adjustment of cholesterol levels, blood sugar, blood pressure)
- Smoking cessation / “What are the benefits of not smoking?”
- Learning relaxation methods
- Improvement of difficulty falling asleep / sleeping through the night
- Improvement of wound healing
- Improvement of the pain situation
- Prevention of a valve infection
Therapy at the GZO
- Diagnostics
Specialist visits, resting ECG, echocardiography, wound assessment, laboratory, exercise ECG with determination of the training heart rate, also for the heart group - Optimization of pharmacotherapy
Most patients continue to require medication even after their aortic valve stenosis has been repaired, be it to thin the blood, to treat any heart failure or cardiac arrhythmia or to control cardiovascular risk factors such as hypercholesterolemia or high blood pressure. Some medications only need to be taken for a limited period of time. - Physical training
Ergometer circulation training, terrain training or Nordic walking, group gymnastics with breathing exercises and everyday training, medical training therapy - Knowledge transfer about the disease
Prevention of valve infection (medical lecture on endocarditis prophylaxis), reduction of risk factors (medical lectures on hypertension, arteriosclerosis, nicotine-free living), coping with anxiety and depression, nutritional advice, diabetes advice - Nutritional advice
All patients receive nutritional advice. Nutritional counseling is available in the form of individual counseling, group counseling and a training kitchen. - Social service
From the organization of home care to the degree of disability to the prescription of assistive devices - Psychocardiology
Learning relaxation methods PMR, Qi Gong, imagination; individual and group discussions if required
What happens at home?
Continuation of moderate endurance training in the THF range (training heart rate), ideally 5×30 min or 3×50 min supplemented by a cardio group, plus moderate strength training and coordination 2-3 per week
Endocarditis prophylaxis with additional professional dental cleaning or check-up twice a year, in the case of diabetes additional medical foot care twice a year
For cardiac insufficiency (heart failure)
Heart failure severely restricts the quality of life with symptoms such as shortness of breath, reduced performance, fatigue and water retention.
Our department is specially designed to focus on heart failure. Well-established treatment concepts are available for systolic heart failure (contraction weakness). However, diastolic heart failure (relaxation weakness) now accounts for a good 50%. Only two drugs are being tested here. What has been proven to help is moderate endurance training, the core competence of rehabilitation. Both groups of heart failure are automatically embedded in our psychocardiology program. We also have a special heart failure group as a follow-up strategy for the outpatient area after inpatient rehabilitation.
After implantation of pacemaker, defibrillator (ICD), CRT
For heart muscle diseases (cardiomyopathies) such as myocarditis
After expired pulmonary embolism
Diseases of the arterial vessels (aorta, neck, pelvic and leg vessels) with stenting or bypass surgery
Analogous to coronary heart disease, these are diseases of arteriosclerosis. The GZO offers special therapy packages for these subtypes, e.g. for peripheral arterial occlusive disease (PAOD) with claudication-guided interval walking training, electrotherapy and manual therapy in addition to optimizing the 10 risk factors of arteriosclerosis.
For cardiac arrhythmias such as atrial fibrillation
For metabolic syndrome with
- High blood pressure
- Diabetes mellitus
- Fat metabolism disorder
- Overweight and obesity
It is often trivialized by calling it affluence syndrome. In fact, it must be described as a deadly quartet, as the risk factors are not added together but multiplied. Once again, the focus is on arteriosclerosis with the optimization of risk factors, above all through the “Poly-Pill” movement
Diagnostics
Qualified cardiac rehabilitation requires comprehensive functional and performance diagnostics of the patient. The determination of physical performance and exercise intensity can be used as part of exercise therapy to assess the training effect and to record and change the patient’s cardiac performance. In addition, a definition of resilience at work and during leisure time, as well as the dose of medication and recommendations or clarification of invasive interventions can be made in collaboration with the cooperating acute hospitals.
The clinic is equipped for these tasks in accordance with the recommendations of the BAR and the German Society for Prevention and Rehabilitation. The following measurements can be taken:
- Multi-channel resting ECG
- Bicycle stress ECG
- 24-hour ECG
- 24-h. Blood pressure measurement
- Transthoracic echocardiography including 3-D, speckle tracking
- Stress echocardiography
- Spiroergometry
- Uni- and bidirectional vascular Doppler sonography
- Color-coded duplex sonography of the vessels
- Rapid tests (troponin, D-dimer, CRP, Sars-Cov-2)
An IMC monitoring unit is available for cardiac emergencies with the option of:
- Continuous heart rhythm monitoring
- Defibrillation
- Intubation
An internal laboratory is available for measuring troponin, D-dimer, blood gases, electrolytes and INR. Further clinical laboratory work is carried out in cooperation with an external laboratory.
Psychocardiology
Depression and other psychosocial stress factors such as social isolation/loneliness have been shown to worsen heart failure(1) and coronary heart disease, but are insufficiently taken into account in everyday clinical practice. Here we have our own specialist area, psychocardiology. Simple tools for everyday life are developed in groups or individual therapy sessions. These are embedded in relaxation techniques such as progressive muscle relaxation, imagination and Qi-Gong. In addition, the social services are involved at an early stage to organize follow-up structures such as “neighbourhood help” and the heart group/heart failure group.
(1) Europ Journal Preventive Caridology (2022, Ladwig)
Heart group/aftercare
What happens at home?
To ensure that what you have learned can be maintained during your inpatient stay, we will refer you to the nearest heart group at the final consultation. Here, the elements of rehabilitation are continued in the group once a week for 90 minutes: Moderate endurance training, moderate strength and coordination training, elements of relaxation and small lectures. Of course, the Oberammergau Health Center has its own heart group. The heart groups are a special concern of Chief Physician Dr. Rosenberger. He is a volunteer on the board of the heart groups. A heart failure group is currently being set up under his leadership.
The heart groups are a special concern of Chief Physician Dr. Rosenberger. He is a volunteer on the board of the heart groups. A heart failure group is currently being set up under his leadership.
During your stay, follow-up appointments will be organized for you or, depending on your medical condition, you will be referred to the GP aftercare programmes for heart attacks and diabetes. Our discharge management team and social services are available to answer any further questions you may have.
Self-help group of the German Heart Foundation in Oberammergau
Scientific work/commitment
INCREASE research project in cooperation with Augsburg University Hospital:
The study (INCREASE) in cooperation with the University of Augsburg has proven that the ERAS concept (Enhanced Recovery after Surgery) is possible in standard care. The study has been running since March 2021. Recruitment and treatment of INCREASE patients at the Oberammergau Health Center has been completed since March 2023. The data collection should be completed by April 2024.
Together with the University of Augsburg, we want to provide scientific proof that our scientific project, the INCREASE concept, enables patients who have undergone heart valve surgery to get back on their feet more gently, with greater self-determination and, above all, much more quickly. This is to be achieved by optimizing the pre-, intra- and post-operative process, not only on an interdisciplinary basis, but also across all sectors.
Preoperative means that interdisciplinary physical exercise, psychological strategy and nutritional optimization ensure that patients are fit for surgery. This is then carried out much more gently. Minimally invasive surgical techniques mean that only a third of the sternum needs to be cut through or the access route is from the side between two ribs. This is made possible by endoscopy technology. Prof. E. Girdauskas at the University of Augsburg is a specialist in this field.
Intra-operative or early post-operative means that the patient is practiced on the IMC on the evening of the operation, then on day 1-4 on the normal ward. On day 5, the patient is transferred to the rehabilitation clinic.
Postoperatively, the cardiology department at the Oberammergau Health Center now comes into play. We can start complex treatment from day 5. Of course, this means that patients arrive at the rehabilitation clinic much earlier and therefore “bloodier”. Of course, the tasks of the acute hospital have to be taken over. No further (muscular) deconditioning occurs due to the early transfer and complex treatment from day 5. On the contrary, at the end of rehab, INCREASE patients have made almost twice as much progress in their treatment compared to standard care. A separate SOP (Standard Operating Procedure) ensures interdisciplinary complex treatment with more precise exercise, psychocardiology, special respiratory therapy and wound experts as well as a scientific assessment. The patient is given an active role right from the start. In addition, relatives are invited to the final visit.
Thanks to the evidence provided, the concept has already been incorporated into standard care. As an ERAS concept, patients will be treated at the Oberammergau Health Center from September 2023.
The next step for the ERAS principle with bypass surgery patients is scheduled for 2024. The Oberammergau Health Center is already registered as a new consortium partner for the INVINITI study. Planned start of studies is July 2024.
Dr. med. Armin Rosenberger
Chief Physician of Cardiology
in February 2024
- Further development of heart groups through voluntary work as a board member of Herz-LAG Bayern (umbrella organization of Bavarian heart groups)
- Establishment of a heart failure group as a contribution to the supra-regional heart failure network.
- Organization of the Oberammergau cardiac sports group in cooperation with TSV Oberammergau
- Cardiac sports groups Bavaria
- Performance diagnostics for the Olympic team of natural track lugers in the German Bobsleigh and Luge Federation (BSD)
- Promotion of junior staff through authorization for further training
events
- Heart Week as an ambassador for the German Heart Week. Heart Foundation
- Lecture University of Augsburg: INREASE from the perspective of rehabilitation
Benefits of cardiac rehabilitation
Cardiac rehabilitation, e.g. for coronary heart disease (heart attack), gives you additional time to live (reduction in mortality). Above all, however, it leads to a reduction in the burden of disease (morbidity) and thus to an increase in your quality of life. This has been proven in several studies. Only in the ideal case is a complete “recovery” possible. The primary aim of rehabilitation measures is to enable people to participate (again) in those situations or areas of life that are important to them (participation) despite their continuing impairments.
At the beginning of the rehabilitation program, (realistic) rehabilitation goals are agreed with you.
Both physical-functional, educational, social-participative and psychological goals are defined.
Examples of this are “being able to climb two flights of stairs again”, “being able to play with the grandchildren again”, “optimizing risk factors such as losing 2 kg of weight”, “dealing with your own vulnerability”.
Goals connect therapist and patient and thus improve the therapy outcome. Goals strengthen self-efficacy and lead to higher overall patient satisfaction.
To achieve all these goals, we work in an interdisciplinary team. This consists of physiotherapists, sports and occupational therapists, doctors and nursing staff, nutritionists, psychologists and social services.
Another focus is on the treatment of risk factors.
All risk factors for arteriosclerosis are treated individually. The patient is guided into an active role through training. This has been proven to prevent secondary events such as another heart attack. The rehabilitation measure lays the foundation for sustainable prevention. To ensure that the health skills acquired during rehabilitation are maintained, we arrange a cardiac group close to home for each patient as a follow-up strategy.


